Authors : Pramod Ingale, Pooja S. K. Rai, Vaishnavi Salunkhe, Poonam Lalla
Conducted at : Biochemistry Department, LTMMC & GH, Sion, Mumbai
Published in : International Journal of Recent Scientific Research
Vol. 12, Issue, 12(B), pp. 43750-43753, December, 2021
Online Link : DOI: https://www.recentscientific.com/study-cardiovascular-risk-thyroid-disorders
ABSTRACT
- Background: Thyroid hormones play an important role in proper functioning of cardiovascular system. The study is to explore the role of lipoprotein in thyroid diseases to find out cardiovascular marker.
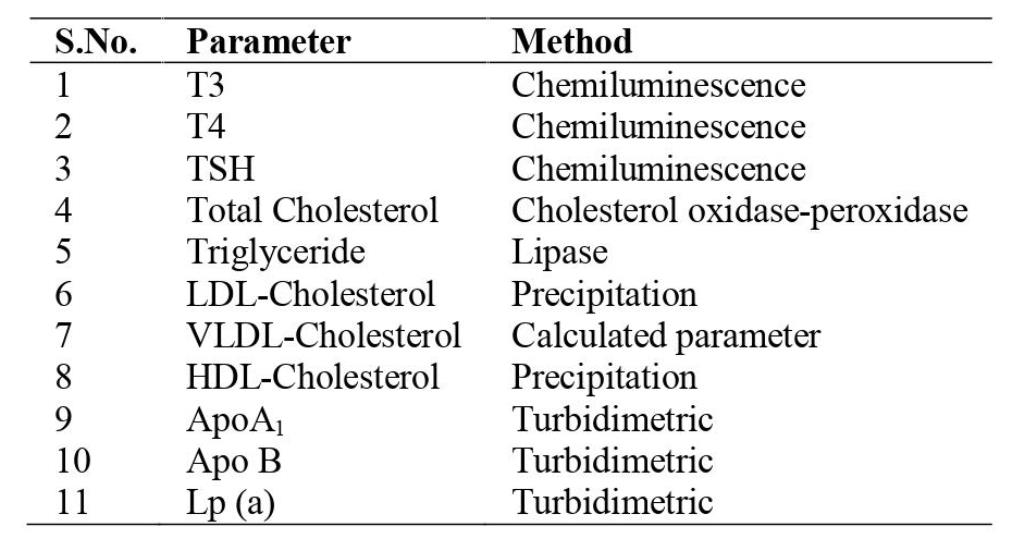
- Subjects and Methods: The study was carried out on 300 samples in clinical biochemistry department. These samples were categorized into 113 hypothyroid, 87 hyperthyroid & 100 age & sex matched euthyroid controls. Serum samples collected and evaluated for triiodothyronine, thyroxine, thyroid-stimulating hormone, total cholesterol, triglyceride (TG), Apolipoprotein A1 (Apo A1), Apolipoprotein B (Apo B), Lipoprotein a Lp(a), low density lipoprotein (LDL), very low density lipoprotein (VLDL) and high-density lipoprotein (HDL).
- Results: 195/300 (65%) suspected patients were suffering from thyroid disorder amongst which 110/195 (56.4%) were hypothyroid and 85/195 (43.6%) were hyperthyroid. The significant increase observed in TG, LDL, Apo A1, Apo B, Lp(a) levels in hypothyroid patients and significant decrease seen in hyperthyroid patients.
- Conclusion: Hyperthyroidism showed abnormal lipid profile with hypercholesterolemia. The evaluation of hypercholesterolemia in thyroid disorder patients recommended with large number of patient numbers.
INTRODUCTION
Thyroid gland is one of the largest endocrine glands in human beings. Thyroid gland secretes iodine containing hormones triiodothyronine (T3) and thyroxine (T4) from thyroid follicular cells which is regulated by the thyroid-stimulating hormone (TSH) secreted by the anterior pituitary gland.(1)Thyroid hormone (TH) regulates metabolic processes essential for normal growth and development as well as regulating metabolism in the adult. (2)Thyroid hormones influence all aspects of lipid metabolism including synthesis, mobilization, and degradation. It promotes both lipolysis and lipogenesis (3,4).Thyroid disease, namely hypothyroidism and hyperthyroidism, constitutes the most common endocrine abnormality worldwide, diagnosed either in subclinical or clinical form. More than 40 million people in India suffer from thyroid diseases. (5)
Dyslipidemia is a common metabolic abnormality in patients with thyroid disease, both in hypothyroidism and hyperthyroidism and constitutes the end result of the effect of thyroid hormones in all aspects of lipid metabolism leading to various quantitative and/or qualitative changes of triglycerides, phospholipids, cholesterol, and other lipoproteins.(6) Thus, this study is carried out to find out cardiovascular risk in Thyroid disorders.
MATERIAL & METHODS
The study was conducted in department of Biochemistry in Lokmanya Tilak Municipal Medical College & Hospital, Mumbai, India. The study was carried out between April 2021 to August 2021 on 300 samples in clinical biochemistry department. These samples were categorized into 113 hypothyroid, 87 hyperthyroid & 100 age & sex matched euthyroid controls. Pregnant women, patients on thyroxine, oral contraceptives, statins, history of rheumatoid arthritis, coronary artery disease, any other acute or chronic inflammatory conditions and patient undergone thyroidectomy were excluded from this study.
The following parameters were analyzed in Biochemistry laboratory using fully automated biochemistry analyzer XL- 640 of Erba Manheim manufactured by Transasia Bio-medicals Ltd. & Chemiluminescence analyzer Access-2 manufactured by Beckmann Coulter Pvt. India Ltd.
Anova test was used to find a significant difference among the groups.
RESULTS
Table 1 Age wise distribution of study subjects
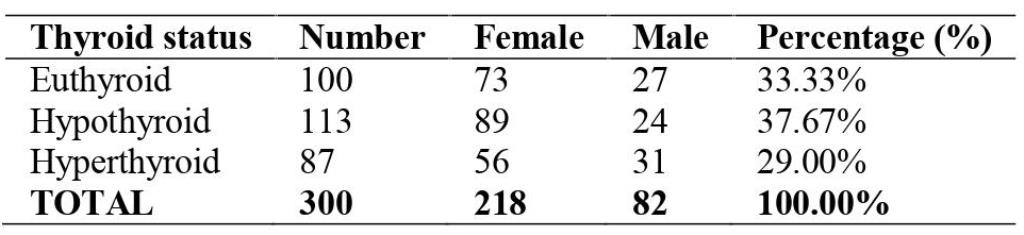
Table 1 shows females (218) were more affected from thyroid disorders than males (82).
Table 2 Levels of T3, T4 & TSH in study groups
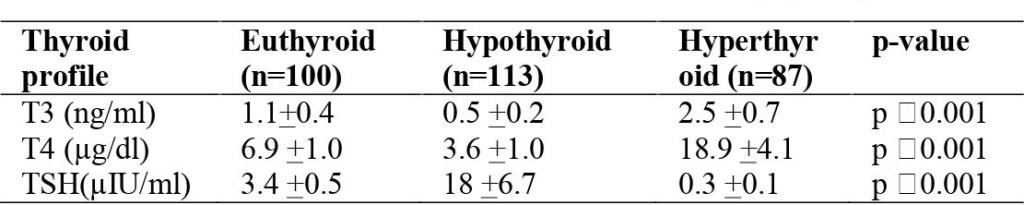
Table 2 shows a significantly (p ˂ 0.001) decreased levels of T3 in the hypothyroid patients (2.5 +0.7) as compared to the healthy controls (1.1+0.4). T4 levels were also significantly (p˂ 0.001) decreased in the hypothyroid patients (3.6+1.0) as compared to the healthy controls (6.9+1.0). There were also a significant (p ˂ 0.001) increases levels of TSH in the hypothyroid patients (18 +6.7) as compared to the healthy individuals (3.4 +0.5).
There is also significant (p ˂ 0.001) increased levels of T3 in the hyperthyroid patients (0.5 ± 0.2) as compared to the healthy controls (1.1+0.4). T4 levels were also significantly (p ˂ 0.001) increased in the hypothyroid patients (18.9 +4.1) as compared to the healthy controls (6.9+1.0). There were also a significant (p ˂ 0.001) decreases levels of TSH in the hyperthyroid patients (0.3 +0.1) as compared to the healthy individuals (3.4 +0.5).
Table 3 Lipid profile& lipoprotein levels in Hypothyroidism & hyperthyroidism
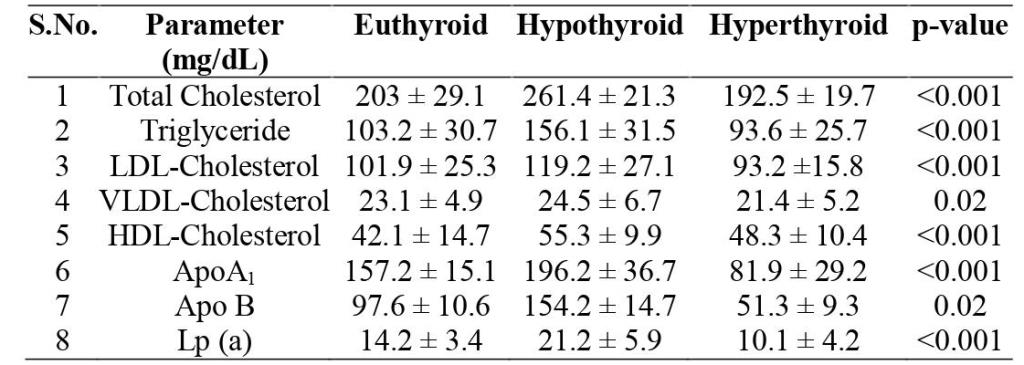
Table 3 shows that there is also significant (p ˂ 0.001) increased levels of Total Cholesterol (261.4 ± 21.3), Triglyceride (156.1 ± 31.5),LDL-Cholesterol (119.2 ± 27.1), HDL-Cholesterol(55.3 ± 9.9) ApoA1(196.2 ± 36.7),Apo B(154.2 ± 14.7), Lp (a)(21.2 ± 5.9) in the hypothyroid patients as compared to the healthy controls (203 ± 29.1,103.2 ± 30.7,101.9 ± 25.3,157.2 ± 15.1,97.6 ± 10.6,14.2 ± 3.4) respectively.
Total Cholesterol (192.5 ± 19.7), Triglyceride (93.6 ± 25.7),LDL -Cholesterol (93.2 ±15.8), ApoA1(81.9 ± 29.2),Apo B (51.3 ± 9.3) & Lp(a)(10.1 ± 4.2) levels in the hyperthyroid patients were decreased as compared to the healthy controls (203 ± 29.1,103.2 ± 30.7,101.9 ± 25.3,157.2 ± 15.1,97.6 ± 10.6, 14.2 ± 3.4) respectively.
DISCUSSION
Hypothyroidism is a common metabolic disorder in the general population. Our study shows increase in levels of Lipid profile & Apo A1, Apo B, Lp(a) in hypothyroid patients.
TC & LDL-C increase levels: This is in accordance with the study done by Pearce et al, Abbas et al, Lee et al that Although decreased thyroid function is accompanied by reduced activity of HMG-CoA reductase causes TC and LDL-C levels to be increased in hypothyroid patients (7-11).Thyroid hormone (TH) increases the synthesis of cholesterol and bile acids (BA) flow, resulting in depletion of hepatic cholesterol and enhancement of cholesterol uptake from the circulation to the liver. By contrast, in hypothyroidism, diminution of TH results in slowing of BA flow, marked diminution in the rate of cholesterol secretion into the bile, increase of intrahepatic cholesterol despite the decrease in cholesterol biosynthesis, and decrease of hepatic uptake of cholesterol from the circulation. This is due to the decreased LDL-receptors activity, resulting in decreased catabolism of LDL and IDL (12).
TG increase levels: Moreover, a decrease in Lipoprotein Lipase activity is found in overt hypothyroidism, decreasing the clearance of TG-rich lipoproteins (13). Therefore, overt hypothyroid patients may also present with elevated TG levels associated with increased levels of VLDL and occasionally fasting chylomicronemia.
VLDL increase levels: The VLDL and IDL particles in hypothyroidism are rich in cholesterol and Apolipoprotein E, thus resembling VLDL particles of type III hyperlipoproteinemia. Therefore, in hypothyroidism, increase in VLDL is because of increase cholesterol and Apolipoprotein E levels. (13)
HDL increase levels: Hypothyroid patients may also exhibit elevated levels of HDL-C mainly due to increased concentration of HDL2 particles. Indeed, due to a reduction of Hepatic Lipase activity a decrease in HDL2 catabolism is observed. Moreover, decreased activity of the CETP results in reduced transfer of cholesteryl esters from HDL to VLDL, thus increasing HDL-C levels.(14-15)
Increased lipoprotein (a) levels: Hypothyroid patients have increased lipoprotein (a) [Lp(a)] levels due to impairment of the catabolism of theapo-B-containing particles, including Lp(a), which are associated with increased CVD risk (16-18).
Cardiovascular risk
The above abnormalities of lipid metabolism associated with hypothyroidism predispose to the development of atherosclerotic coronary artery disease (CAD). Moreover, hypothyroidism can adversely affect other CVD risk factors, further contributing to increasing CAD risk. Decreased thyroid function not only increases the number of LDL particles, but also promotes LDL oxidation. Elevated plasma concentrations of Lp(a), as found in hypothyroid subjects, could accelerate the development of atherosclerosis by several mechanisms. The apo(a) moiety may promote the association of LDL to the surface of cells by a receptor-independent mechanism, or Lp(a) can bind to glycosaminoglycans in the vessel wall and become a target for migrating macrophages. In the hypothyroid state, glycosaminoglycans accumulate in several tissues. (19)
Furthermore, hypothyroidism increases plasma homocysteine levels, which can be attributed to the hypothyroidism-induced decline of kidney function as well as impaired methylenetetrahydrofolate reductase activity. In addition, thyroid failure is strongly associated with arterial hypertension (especially diastolic) via sympathetic and adrenal activation and increased vascular stiffness (20-21).
Hyperthyroidism
The incidence of hyperthyroidism is lower (2.2%) compared with hypothyroidism in the general population. (22)
Despite the increased activity of the HMG-CoA reductase, levels of TC, LDL-C, ApoB and Lp(a) tend to decrease in patients with hyperthyroidism. This is due to increased LDL receptor gene expression resulting in enhanced LDL receptor- mediated catabolism of LDL particles. Furthermore, hyperthyroidism results in enhanced LDL oxidation, which is related to FT4 levels. A decrease in HDL-C levels is also observed in hyperthyroidism, due to increased CETP-mediated transfer of cholesteryl esters from HDL to VLDL and increased Hepatic Lipase-mediated catabolism of HDL2.(23-24)
Triglyceride levels remain unchanged. The decrease in Lp(a) concentrations during hyperthyroidism could also be mediated by increased activity of the LDL-C receptor. (25)
CONCLUSION
In this study, in thyroid disorders, the values of LDL, HDL, TG, Apo A1, Lp(a)and cholesterol are significantly deranged. Thus, in these patients’ lipid & lipoprotein levels can be used as cardiovascular risk marker. However, further studies with a greater number of hypercholesterolemic patients and other thyroid disorder are recommended.
Bibliography
- Hall JE, Guyton AC (2011). Guyton and Hall textbook of medical physiology (12th ed.). Philadelphia, Pa.: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
- Mullur, R., Liu, Y.-Y., & Brent, G. A. (2014). Thyroid Hormone Regulation of Metabolism. Physiological Reviews,94(2),355–382. doi:10.1152/physrev.00030.2013
- Liu YY, Brent GA. Thyroid hormone crosstalk with nuclear receptor signaling in metabolic regulation. Trends Endocrinol Metab 21: 166–173, 2010.
- Webb P. Thyroid hormone receptor and lipid regulation. CurrOpin Invest Drugs 11: 1135–1142, 2010.
- G. Unnikrishnan & U. V. Menon; Thyroid disorders in India: An epidemiological perspective; Indian J Endocrinol Metab. 2011 Jul; 15(Suppl2): S78–S81.
- X. Zhu and S. Y. Cheng, “New insights into regulation of lipid metabolism by thyroid hormone,” Current Opinion in Endocrinology, Diabetes and Obesity, vol. 17, no. 5, pp. 408–413, 2010.
- Pearce EN, Wilson PW, Yang Q, Vasan RS, Braverman LE. Thyroid function and lipid sub particle sizes in patients with short term hypothyroidism and a population-based cohort. J Clin Endocrinol Metab 2008; 93: 888-94.
- Abbas JM, Chakraborty J, Akanji AO, Doi SA. Hypothyroidism results in small dense LDL independent of IRS traits and hypertriglyceridemia. Endocr J 2008; 55: 381-9.
- Al-Tonsi AA, Abdel-Gayoum AA, Saad M. The secondary dyslipidemia and deranged serum phosphate concentration in thyroid disorders. Exp Mol Pathol 2004; 76: 182-7.
- Teixeira Pde F, Reuters VS, Ferreira MM, et al. Lipid profile in different degrees of hypothyroidism and effects of levothyroxine replacement in mild thyroid failure. Transl Res 2008; 151: 224-31.
- Lee WY, Suh JY, Rhee EJ, Park JS, Sung KC, Kim SW. Plasma CRP, apolipoprotein A-1, apolipoprotein B and Lp(a) levels according to thyroid function status. Arch Med Res 2004; 35: 540-5.
- Leonidas H. Duntas, Gabriela Brenta.A Renewed Focus on the Association Between Thyroid Hormones and Lipid Metabolism.Front Endocrinol 2018; 9:511.
- Nikkila EA, Kekki M. Plasma triglyceride metabolism in thyroid disease. J Clin Invest 1972; 51: 2103-14.
- Lam KS, Chan MK, Yeung RT. High-density lipoprotein cholesterol, hepatic lipase and lipoprotein lipase activities in thyroid dysfunction--effects of treatment. Q J Med 1986; 59: 513- 21.
- Dullaart RP, Hoogenberg K, Groener JE, Dikkeschei LD, Erkelens DW, Doorenbos H. The activity of cholesteryl ester transfer protein is decreased in hypothyroidism: a possible contribution to alterations in high-density lipoproteins. Eur J Clin Invest 1990; 20: 581-7.
- de Bruin TW, van Barlingen H, van Linde-Sibenius Trip M, van Vuurst de Vries AR, Akveld MJ, Erkelens DW. Lipoprotein (a) and apolipoprotein B plasma concentrations in hypothyroid, euthyroid, and hyperthyroid subjects. J Clin Endocrinol Metab 1993; 76: 121- 6.
- Tzotzas T, Krassas GE, Konstantinidis T, Bougoulia M. Changes in lipoprotein(a) levels in overt and subclinical hypothyroidism before and during treatment. Thyroid 2000; 10: 803-8.
- Klausen IC, Nielsen FE, Hegedus L, Gerdes LU, Charles P, Faergeman O. Treatment of hypothyroidism reduces low-density lipoproteins but not lipoprotein(a). Metabolism 1992; 41: 911-4.
- de Bruin, T W; van Barlingen, H; van Linde-Sibenius Trip, M; van Vuurst de Vries, A R; Akveld, M J;Erkelens, D W .Lipoprotein(a) and apolipoprotein B plasma concentrations in hypothyroid, euthyroid, and hyperthyroid subjects.. The Journal of Clinical Endocrinology & Metabolism 1993; 76(1):121–6.
- Tunbridge WM, Evered DC, Hall R, et al. Lipid profiles and cardiovascular disease in the Whickham area with particular reference to thyroid failure. Clin Endocrinol (Oxf) 1977; 7: 495- 508.
- Pucci E, Chiovato L, Pinchera A. Thyroid and lipid metabolism. Int J ObesRelatMetabDisord 2000; 24(Suppl 2): S109-12.
- Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med 2000; 160: 526- 34.
- Kung AW, Pang RW, Lauder I, Lam KS, Janus ED. Changes in serum lipoprotein(a) and lipids during treatment of hyperthyroidism. Clin Chem 1995; 41: 226- 31.
- Aviram M, Luboshitzky R, Brook JG. Lipid and lipoprotein pattern in thyroid dysfunction and the effect of therapy. Clin Biochem 1982; 15: 62-6.
- Engler, H; Riesen, W F. Effect of thyroid function on concentrations of lipoprotein (a). Clinical Chemistry 1993; 39(12) :2466–9.